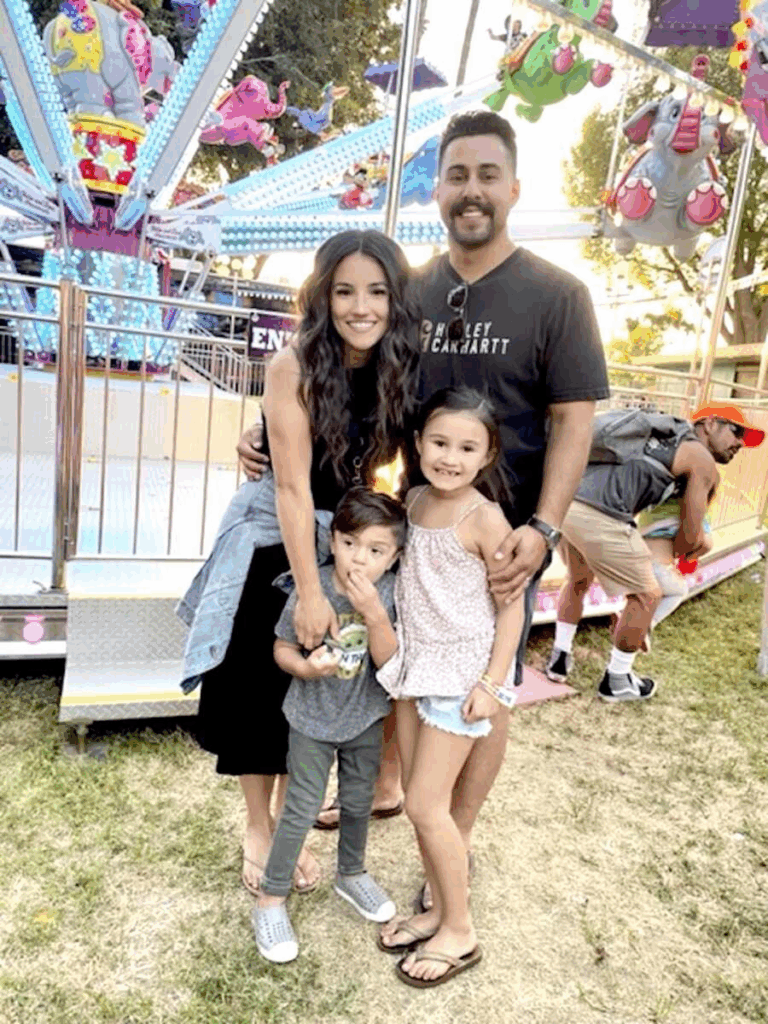
Their daughter gave her brother the cells he needed to live, and in doing so, she gave their whole family a future to grow into together. Kelsey is a wife and mom to two kids, Olivia, six, and Eli, four. When Eli was born, life felt beautifully balanced: one daughter, one son, a happy big sister who adored her baby brother. Then minor, puzzling signs began to stack up. Eli’s belly stayed enlarged. He snored and breathed loudly. His head and tongue were huge, swallowing was hard, one eye looked cloudy, and a tiny hump appeared on his lower back.

His baby teeth came in out of order, crawling took longer, and he had an umbilical hernia. None of it seemed alarming alone, but together it was a lot. At his nine-month checkup, the pediatrician suggested genetic testing “just to cover bases.” Kelsey didn’t feel worried; Eli was cheerful and had no family history to point to. Six weeks later, a doctor called with results: Mucopolysaccharidosis type 1, MPS I. The word “fatal” slipped into the conversation, and everything blurred.

That night, she and her husband read the email together, and in minutes, they knew their world had changed. She sat by Eli’s crib, holding his tiny hand, crying quietly in the dark, trying to understand what the future would be. They learned MPS is a rare disorder where the body lacks a key enzyme. There are six types; Eli had MPS I, the most severe form, Hurler syndrome. The hard truth was that it’s the worst kind to have; the hopeful news was that the most aggressive, effective treatments are aimed at it.
Step one: weekly 6–8 hour enzyme infusions to slow regression. Then nine days of intense chemotherapy, followed by a bone marrow transplant to give his body donor cells that could make the missing enzyme. They chose the University of Minnesota Masonic Children’s Hospital, the global leader in MPS transplants, even though they lived in Orange County, California. After seven preparatory surgeries and a short recovery at home, Kelsey packed for five months in Minnesota with both kids while her husband returned to work. The Ronald McDonald House became their safe landing pad.

Next came the search for a donor. Parents are usually only 50% matches, so doctors first tested Olivia. Backup matches were found in cord blood banks, six near-perfect options, but a matched sibling would be best. The call came: Olivia was a 10/10 perfect match. Kelsey explained what it meant, and her four-year-old didn’t hesitate: “Yes, Mom, I want to help him.”
Eli began twice-daily chemo for nine straight days. On day ten, it was transplant time. Kelsey walked Olivia into the operating room and held her hands as she fell asleep. Surgeons drew marrow from both hip bones, filtered it, and rolled it into Eli’s room in two crimson bags. Kelsey and her husband watched as the nurse connected the line and he released the clamp. In twenty quiet minutes, their daughter’s cells began a new job inside their son.
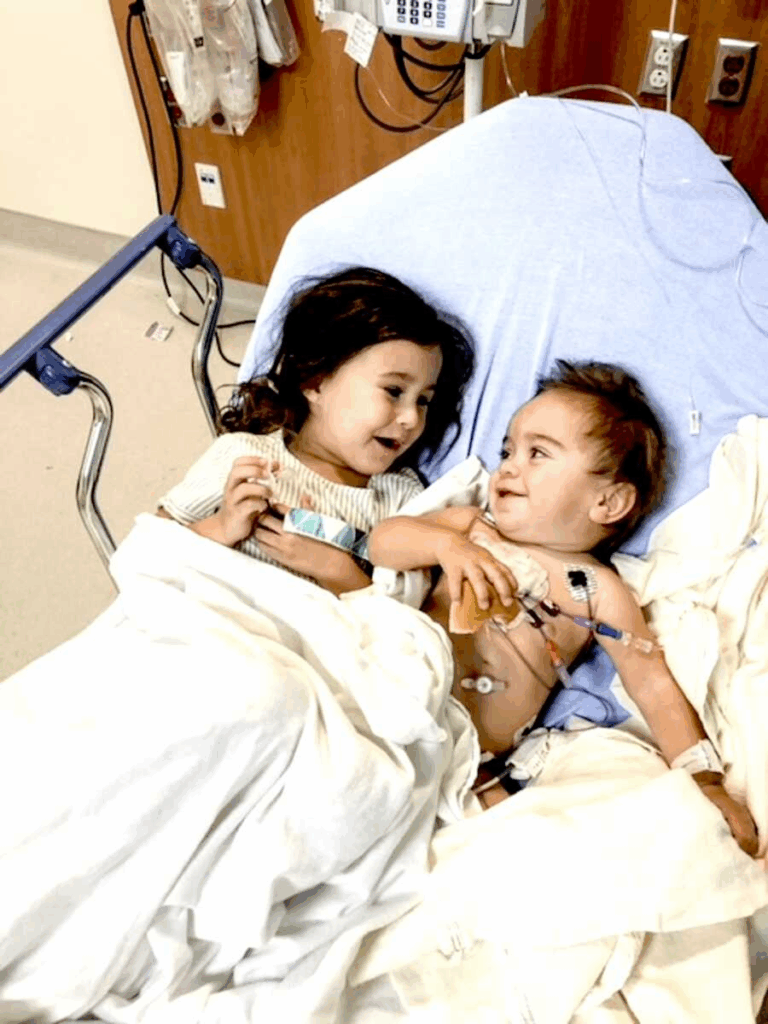
Complications can hit hard after a transplant. Kelsey’s husband returned home, and she managed the long watch with both kids. Eli had a few short-lived chemo side effects; his hair fell out, and he got his first haircut on the hospital floor. Then his blood counts started climbing, every day, a little more. On day 21, far earlier than most, he was strong enough to leave the BMT unit and return to the Ronald House. They still had to stay within minutes of the hospital for at least 100 days, with frequent checks, but they were out of the four walls that had held so much fear.

They made a life in the in-between: new friends, snow days, holidays away from home, sister and brother side by side. When the 100-day mark arrived with excellent numbers, doctors cleared them to go home. Eli had one more surgery to switch his central lines to a long-term port, and then Kelsey arranged their trip. Because of Eli’s fragile immune system, Aero Angel provided private flights. The family met them on the plane with a welcome-home sign and tears.
The first year back was careful and quiet. Eli continued weekly enzyme infusions for a time, but infections twice forced removal of the port, and they chose not to replace it. There is no cure for MPS, so they return to Minnesota every year for complete evaluations. Eli’s reports have been good twice now. There are no new concerns, steady progress, and hopeful futures. The most important number is engraftment: how much of his marrow is his donor’s. The doctor called this January while driving to the airport after his two-year check. Eli is still 100% Olivia on the inside. That’s why he’s thriving.

Olivia and Eli are best friends. Their parents never forget the sight of their daughter’s cells flowing into their son’s body, the moment two siblings, already close, became connected in a way most families never witness. They’re grateful for doctors, the Ronald House, Aero Angel, and everyone who stood with them. Mostly, they’re thankful for a brave little girl who said “yes” without blinking, and a little boy who stayed joyful through the hardest days.