Two tiny girls taught their mother that miracles don’t arrive tidy; they storm in, sirens blazing, and leave you braver than you ever planned to be. She’s a private person by nature, but the road to her twins felt too hard-won to keep quiet. She married Stan at 25, childhood classmates who found each other again, and figured that starting a family would be simple. It wasn’t. Month after month, 2017 brought disappointment, followed by two early positives that faded into chemical pregnancies. Bloodwork, scans, a specialist, even a laparoscopy: every test said she was “perfect.” Still, nothing.

In December, she tried again after a trigger shot. On New Year’s Eve, a bold line stared back. This time, the HCG rose, but her progesterone slipped. She spent weeks inserting progesterone pessaries, shuffling between labs and appointments, counting days to the first scan. At eight weeks, she lay on the table, braced for silence. A heartbeat whooshed through the room.
Then the doctor frowned, shifted the probe, and said there were two. Shock rattled them both; she shook; Stan turned white and had to step outside. The relief was short; the twins shared a placenta (MCDA) and looked so close together that the second heartbeat was nearly missed. Complications were possible, including twin-to-twin transfusion syndrome. Five days later, another scan showed two transparent sacs and proper dates. They exhaled.

Because the pregnancy was high-risk, she transferred to a twin specialist. Fortnightly scans became their rhythm. She felt lucky; she had no morning sickness, just bone-deep fatigue. Work tapered off at 19 weeks when fluid changes appeared around one baby’s sac; she stopped completely by 22 weeks to protect against early labor. At 29 weeks, a Doppler showed early signs of TTTS. She had steroid shots and back-to-back checks that wavered between “looks okay” and “not happy.” Then came the call no mother wants: her hospital couldn’t take babies under 32 weeks. Bags already packed, she was sent to Mercy Hospital, away from her doctor, her routine, and her comfort zone.
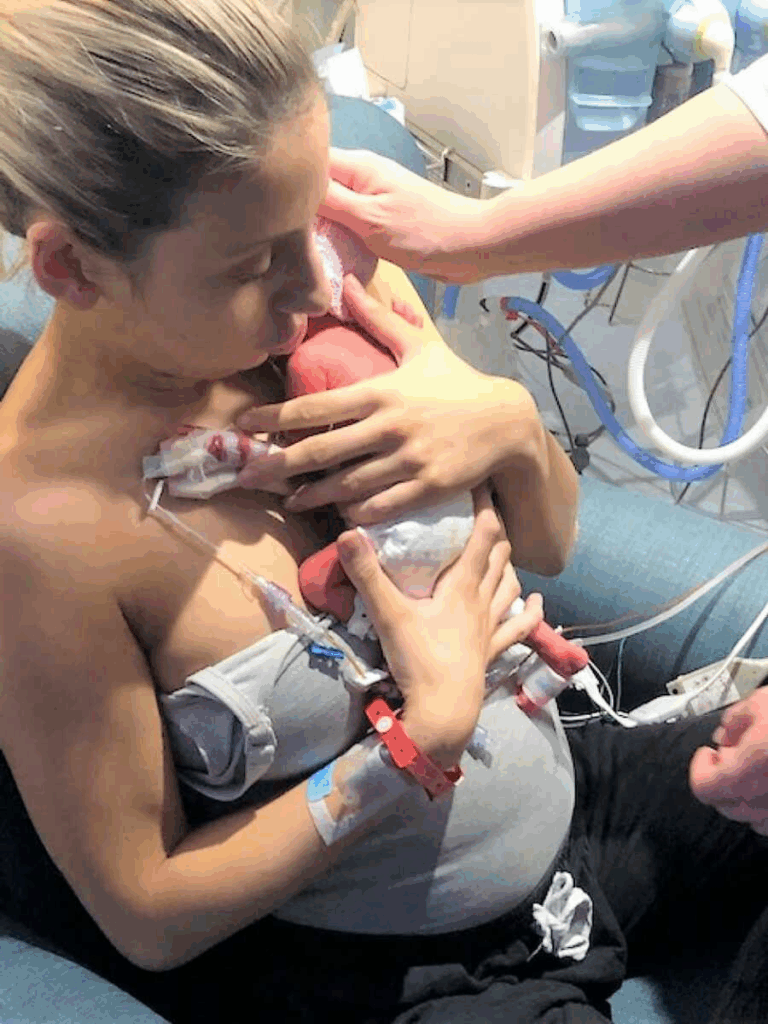
At 30 weeks and 3 days, on July 8, Tia and Victoria arrived by emergency C-section, each just over two and a half pounds. Tia went straight to the NICU; her mother held Victoria for seconds before she, too, was whisked away. The days that followed were a grind of alarms, tubes, two-hourly pumping, and 12- to 14-hour bedside vigils. Two weeks later they were transferred closer to home. The scare didn’t end. A 4 a.m. call reported Tia had influenza and bronchitis and was on breathing support. Victoria battled two staph infections and IV antibiotics. Their parents watched tiny chests work for every breath and felt helpless in ways they’d never imagined.
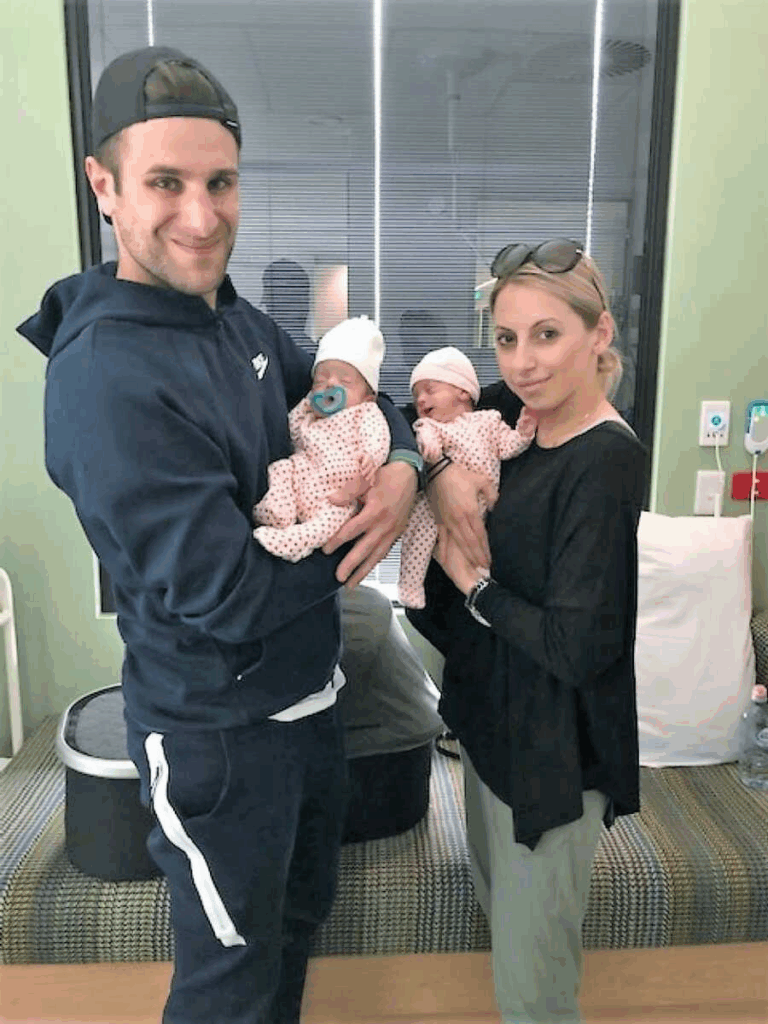
Slowly, the tide turned. Weight crept up. Monitors quieted. On September 2 they finally carried both daughters through their own front door. The gratitude was enormous, toward the nurses who taught them how to touch a baby around wires, the doctors who made fast calls, the hospitals that caught them when plans fell through. Today Tia and Victoria are energetic, opinionated two-and-a-half-year-olds who adore Peppa Pig and each other, proof that the most fragile beginnings can lead to loud, joyful lives.
She looks back on the years of “perfect” test results, the fear in the elevator after “two heartbeats,” the transfer she didn’t want, the NICU nights that stole her breath, and sees a thread running through all of it: stubborn hope. The kind that keeps you taking one more pill, one more scan, one more step into yet another unknown.